Preparing for a Smallpox Bioterrorist Attack: Pulse Vaccination as an Optimal Strategy
Background
At the height of the US invasion of Iraq, bioterrorism was a real and urgent concern. In particular, many feared that laboratory strains of the smallpox virus—a virus that had been eradicated in 1979—had reached the wrong hands and would be used to devastating effect. Thus, in mid-2003 the Israeli Ministry of Health initiated a collaboration with IMBM to attempt to determine the optimal vaccination policy for dealing with a smallpox bioterrorist attack.
Previous studies had attempted to model and assess the efficacy and costs of the following smallpox vaccination strategies:
- Preliminary vaccination: vaccination of the entire population (or parts of it) before an attack.
- One-time mass vaccination: vaccination of the entire population immediately after an attack.
- Ring vaccination: vaccination and isolation of close contacts of individuals suspected of having been exposed to the virus.
Unfortunately, these studies produced conflicting results, possibly because they all made different assumptions about how the smallpox virus would behave in a contemporary population. Additionally, previous studies did not take into account long-term effects of an outbreak, despite the fact that infectious diseases such as smallpox have periodic dynamics: after an outbreak, incidence of the disease soon diminishes to undetectable levels owing to herd immunity; however, epidemics (of diminishing potency) still recur every few years as new, susceptible individuals enter the population.
Methods
We examined a new vaccination approach that takes into account the periodic dynamics of smallpox epidemiology. This approach, called pulse vaccination, involves vaccination of small parts of the population at specified intervals after the attack.
We compared the pulse vaccination strategy with preliminary vaccination and with one-time mass vaccination. Ring vaccination was not examined, as it is not considered a feasible policy in Israel owing to the country’s small geographic size and high population density.
We evaluated strategy efficacy using a weighted cost function that incorporated parameters such as the number of deaths by infection and the number of deaths resulting from vaccination. (The smallpox vaccinia vaccine may cause side effects, some of which can be fatal.) We also tested a broad range of disease-related parameters to ensure that our results would be robust to varying potency of the smallpox virus.
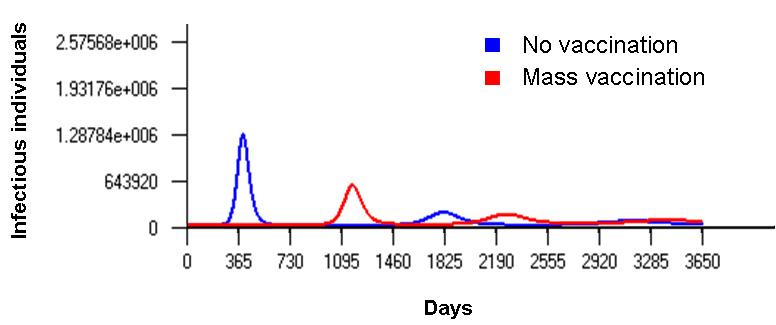
Figure 1
Dynamics of smallpox infection in a population, with or without one-time mass vaccination. Although one-time mass vaccination can prevent an epidemic immediately after disease outbreak, epidemics are likely to resurface several years later.
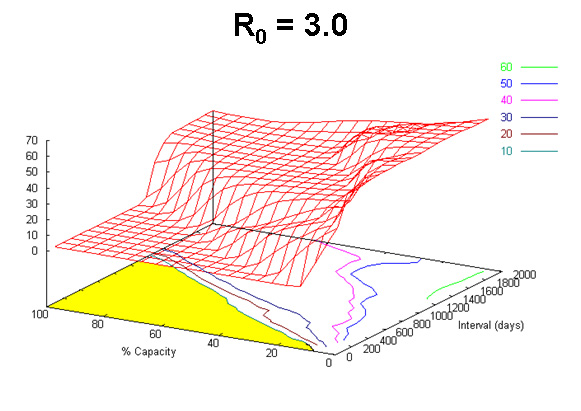
Figure 2
“Cost” as a function of the number of people vaccinated (% capacity, i.e. the percentage of vaccination capacity used) and the interval between “pulse” campaigns for a given disease transmission rate. There is a critical ratio between the number of people vaccinated and the interval between pulses below which cost is zero (shaded area).
Results and Conclusions
Our simulations showed that pulse vaccination was significantly more effective than preliminary or one-time mass vaccination in preventing recurring smallpox outbreaks. Furthermore, we observed that for the pulse strategy to be effective, a critical ratio between the number of vaccinees and the interval between “pulses” (vaccination campaigns) must be maintained.
For further reading
- Agur, Z. Marron, K., Shai, H., Danon, Y. L. Preparing for a smallpox bioterrorist attack: pulse vaccination as an optimal strategy. In M. S. Green et al. (Eds.), Risk Assessment and Risk Communication Strategies in Bioterrorism Preparedness. 2007, pp. 219–229. Dordrecht, The Netherlands: Springer.